Research
A comprehensive listing of our published research may be found on PubMed or Google Scholar . Below are key papers by scientific area to summarize the major themes across the research portfolio.
Methods and Software for Infectious Disease Modeling
My methodological research centers on developing generalized methods and software tools for modeling infectious disease transmission dynamics. This has included EpiModel, a software platform with tools for building and simulating these models. I am the lead author and developer of this software. EpiModel specializes in network-based epidemic modeling using the statistical framework of exponential random graph models, a flexible and robust approach to representing dynamic contact structures. Our methods have been formalized and described in a scientific journal article. The EpiModel platform is fully open-source and available in a Github respository, meaning external researchers can freely access this tool and extend our source code for novel research purposes. This is facilitated with a comprehensive online presence. My team further supports EpiModel users with Network Modeling for Epidemics (NME), an annual workshop at the University of Washington, with training materials also available freely online.
Representative Publications
Jenness SM, Goodreau SM and Morris M. EpiModel: An R Package for Mathematical Modeling of Infectious Disease over Networks. Journal of Statistical Software. 2018; 84(8): 1-47.

Abstract. Package EpiModel provides tools for building, simulating, and analyzing mathematical models for the population dynamics of infectious disease transmission in R. Several classes of models are included, but the unique contribution of this software package is a general stochastic framework for modeling the spread of epidemics on networks. EpiModel integrates recent advances in statistical methods for network analysis (temporal exponential random graph models) that allow the epidemic modeling to be grounded in empirical data on contacts that can spread infection. This article provides an overview of both the modeling tools built into EpiModel, designed to facilitate learning for students new to modeling, and the application programming interface for extending package EpiModel, designed to facilitate the exploration of novel research questions for advanced modelers.
Empirical Data Collection and Bias Analysis to Support Modeling
My applied infectious disease modeling is grounded in the philosophy that good models depend upon good data. I have extensive experience developing and executing empirical studies to generate descriptive data points directly useful for model parameterization. A recent highlight of this effort is the ARTnet study of MSM in the United States, for which my team has generated epidemiological comparisons of the key sexual partnership network features critical for transmission, as well as clinical features also used in models (also involving a web app to facilitate parameterization). Several new studies (see active research support), such as ePrEP, have integrated my network surveys into their study tools for direct use in modeling aims for those projects. Data from these studies have also been evaluated for bias, as in a recent report with longitudinal cohort data on networks.
Representative Publications
Weiss KM, Goodreau SM, Morris M, Prasad P, Ramaraju R, Sanchez T, Jenness SM. Egocentric Sexual Networks of Men Who Have Sex with Men in the United States: Results from the ARTnet Study. Epidemics. 2020; 30: 100386.
 Abstract. In this paper, we present an overview and
descriptive results from one of the first egocentric network studies of
men who have sex with men (MSM) from across the United States: the
ARTnet study. ARTnet was designed to support prevention research for
human immunodeficiency virus (HIV) and other sexually transmitted
infections (STIs) that are transmitted across partnership networks.
ARTnet implemented a population-based egocentric network study design
that sampled egos from the target population and asked them to report on
the number, attributes, and timing of their sexual partnerships. Such
data provide the foundation needed for parameterizing stochastic network
models that are used for disease projection and intervention planning.
ARTnet collected data online from 2017 to 2019, with a final sample of
4904 participants who reported on 16198 sexual partnerships. The aims of
this paper were to characterize the joint distribution of three network
parameters needed for modeling: degree distributions, assortative
mixing, and partnership age, with heterogeneity by partnership type
(main, casual and one-time), demography, and geography. Participants had
an average of 1.19 currently active partnerships (“mean degree”), which
was higher for casual partnerships (0.74) than main partnerships (0.45).
The mean rate of one-time partnership acquisition was 0.16 per week
(8.5 partners per year). Main partnerships lasted 272.5 weeks on
average, while casual partnerships lasted 133.0 weeks. There was strong
but heterogenous assortative mixing by race/ethnicity for all groups.
The mean absolute age difference for all partnership types was 9.5
years, with main partners differing by 6.3 years compared to 10.8 years
for casual partners. Our analysis suggests that MSM may be at sustained
risk for HIV/STI acquisition and transmission through high network
degree of sexual partnerships. The ARTnet network study provides a
robust and reproducible foundation for understanding the dynamics of
HIV/STI epidemiology among U.S. MSM and supporting the implementation
science that seeks to address persistent challenges in HIV/STI
prevention.
Abstract. In this paper, we present an overview and
descriptive results from one of the first egocentric network studies of
men who have sex with men (MSM) from across the United States: the
ARTnet study. ARTnet was designed to support prevention research for
human immunodeficiency virus (HIV) and other sexually transmitted
infections (STIs) that are transmitted across partnership networks.
ARTnet implemented a population-based egocentric network study design
that sampled egos from the target population and asked them to report on
the number, attributes, and timing of their sexual partnerships. Such
data provide the foundation needed for parameterizing stochastic network
models that are used for disease projection and intervention planning.
ARTnet collected data online from 2017 to 2019, with a final sample of
4904 participants who reported on 16198 sexual partnerships. The aims of
this paper were to characterize the joint distribution of three network
parameters needed for modeling: degree distributions, assortative
mixing, and partnership age, with heterogeneity by partnership type
(main, casual and one-time), demography, and geography. Participants had
an average of 1.19 currently active partnerships (“mean degree”), which
was higher for casual partnerships (0.74) than main partnerships (0.45).
The mean rate of one-time partnership acquisition was 0.16 per week
(8.5 partners per year). Main partnerships lasted 272.5 weeks on
average, while casual partnerships lasted 133.0 weeks. There was strong
but heterogenous assortative mixing by race/ethnicity for all groups.
The mean absolute age difference for all partnership types was 9.5
years, with main partners differing by 6.3 years compared to 10.8 years
for casual partners. Our analysis suggests that MSM may be at sustained
risk for HIV/STI acquisition and transmission through high network
degree of sexual partnerships. The ARTnet network study provides a
robust and reproducible foundation for understanding the dynamics of
HIV/STI epidemiology among U.S. MSM and supporting the implementation
science that seeks to address persistent challenges in HIV/STI
prevention.
Jenness SM, Weiss KM, Prasad P, Zlotorzynska M, Sanchez T. Bacterial STI Screening Rates by Symptomatic Status among Men Who Have Sex with Men in the United States: A Hierarchical Bayesian Analysis. Sexually Transmitted Diseases. 2019; 46(1): 25–30.
 Background. Prevention of bacterial sexually
transmitted infections (STIs) among men who have sex with men (MSM)
requires timely disease detection, but this is complicated by
asymptomatic infection. We estimated screening/testing rates by
symptomatic status to evaluate adherence to Centers for Disease Control
and Prevention STI screening guidelines.
Background. Prevention of bacterial sexually
transmitted infections (STIs) among men who have sex with men (MSM)
requires timely disease detection, but this is complicated by
asymptomatic infection. We estimated screening/testing rates by
symptomatic status to evaluate adherence to Centers for Disease Control
and Prevention STI screening guidelines.
Methods. In a cross-sectional study of 2572 US MSM aged 15 to 65 years in 2017 to 2018, we measured the reported number of asymptomatic STI screens in the past 2 years versus tests prompted by disease symptoms. Using negative binominal regression within a hierarchical Bayesian framework, we estimated yearly rates of asymptomatic screening and symptomatic testing by geographic, demographic, and behavioral factors.
Results. Human immunodeficiency virus (HIV) status was most strongly associated with all testing/screening frequency (incidence rate ratio [IRR], 1.72; 95% credible interval [Crl], 1.49, 1.97). The HIV-uninfected MSM had 0.14 (95% credible interval [CrI], 0.12-0.17) symptomatic tests and 0.88 (95% CrI, 0.77-1.01) asymptomatic screens per year. The HIV-infected MSM had 0.25 (95% CrI, 0.18-0.35) symptomatic tests and 1.53 (95% CrI, 1.24-1.88) asymptomatic screens per year. Rates of asymptomatic screening were higher among black compared with white MSM (IRR, 1.41; 95% CrI, 1.15-1.73), but weakly associated with number of past-year sexual partners (IRR, 1.01; 95% CrI, 1.00-1.01). Overall, 85% to 90% of diagnostic events were asymptomatic screens.
Conclusions. Self-reported rates of STI screening were close to Centers for Disease Control and Prevention's recommended overall annual screening frequency, but with gaps defined by demographics and behavioral risk. Targeted screening efforts may be indicated specifically for younger MSM and those with multiple partners.
Shiny Web AppSiegler A, Brock JB, Hurt CB, Ahlschlager L, Dominguez K, Kelley C, Jenness SM, Wilde G, Jameson S, Bailey-Herring G, Mena LA. An Electronic Pre-Exposure Prophylaxis Initiation and Maintenance Home Care System for Nonurban Young Men Who Have Sex With Men: Protocol for a Randomized Controlled Trial. Journal of Medical Internet Research, Research Protocols. 2019; e13982.
 Background. Pre-exposure prophylaxis (PrEP) is highly
efficacious for preventing HIV but has not yet been brought to scale
among at-risk persons. In several clinical trials in urban areas,
technology-based interventions have shown a positive impact on PrEP
adherence. In rural and small-town areas in the United States, which
often do not have geographically proximal access to PrEP providers,
additional support may be needed. This may be particularly true for
younger persons who are more likely to face multiple barriers to
accessing PrEP services. Home-based care, accomplished through a
tailored mobile phone app, specimen self-collection (SSC), and
interactive video consultations, could increase both PrEP initiation and
persistence in care.
Background. Pre-exposure prophylaxis (PrEP) is highly
efficacious for preventing HIV but has not yet been brought to scale
among at-risk persons. In several clinical trials in urban areas,
technology-based interventions have shown a positive impact on PrEP
adherence. In rural and small-town areas in the United States, which
often do not have geographically proximal access to PrEP providers,
additional support may be needed. This may be particularly true for
younger persons who are more likely to face multiple barriers to
accessing PrEP services. Home-based care, accomplished through a
tailored mobile phone app, specimen self-collection (SSC), and
interactive video consultations, could increase both PrEP initiation and
persistence in care.
Objective. The goal of this study is to assess the initiation and persistence in PrEP care for those randomized to a home-care intervention (electronic PrEP, ePrEP) relative to those assigned to the standard of care (control) condition. We will conduct additional assessments, including quantitative and qualitative analyses, to contextualize trial results and facilitate scale-up.
Methods. This 2-arm, randomized controlled trial will enroll young men who have sex with men (YMSM) aged between 18 and 24 years from rural areas of Georgia, Mississippi, and North Carolina. The trial will seek to recruit a diverse sample, targeting 50% participation among highly impacted groups of black or Latino men who have sex with men. Intervention participants will receive a study app that incorporates a messaging platform, a scheduling and milestone-based tracking system for PrEP care progress, electronic behavioral surveys, and interactive video consultations with a clinician. Complemented by SSC kits mailed to laboratories for standard PrEP-related monitoring, the ePrEP system will allow participants to access PrEP care without leaving their homes. YMSM randomized to the control condition will receive a listing of nearest local PrEP providers to receive standard PrEP care. Both groups will complete quarterly electronic surveys. The primary outcome, assessed at 6 and 12 months after randomization, will be the difference in the proportion of intervention versus control participants that achieve protective levels of the active metabolite of oral PrEP (tenofovir diphosphate in dried blood spots).
Results. Enrollment will begin in May 2019, with study completion in 2022.
Conclusions. This trial will determine whether home PrEP care provided through an app-based platform is an efficacious means of expanding access to PrEP care for a diverse group of YMSM in rural and small-town areas of the United States.
Uong S, Rosenberg ES, Luisi N, Goodreau SM, Sullivan PS, Jenness SM. Assessing the Validity of Sexual Network Degree among Men Who Have Sex with Men using Prospective Cohort Data. Epidemiology. 2020; 31(2): 229-237.
 Background. Sexual network degree, a count of ongoing
partnerships, plays a critical role in the transmission dynamics of
human immunodeficiency virus and other sexually transmitted infections.
Researchers often quantify degree using self-reported cross-sectional
data on the day of survey, which may result in bias because of
uncertainty about future sexual activity.
Background. Sexual network degree, a count of ongoing
partnerships, plays a critical role in the transmission dynamics of
human immunodeficiency virus and other sexually transmitted infections.
Researchers often quantify degree using self-reported cross-sectional
data on the day of survey, which may result in bias because of
uncertainty about future sexual activity.
Methods. We evaluated the bias of a cross-sectional degree measure with a prospective cohort study of men who have sex with men (MSM). At baseline, we asked men about whether recent sexual partnerships were ongoing. We confirmed the true, ongoing status of those partnerships at baseline at follow-up. With logistic regression, we estimated the partnership-level predictors of baseline measure accuracy. With Poisson regression, we estimated the longitudinally confirmed degree as a function of baseline predicted degree.
Results. Across partnership types, the baseline ongoing status measure was 70% accurate, with higher negative predictive value (91%) than positive predictive value (39%). Partnership exclusivity and racial pairing were associated with higher accuracy. Baseline degree generally overestimated confirmed degree. Bias, or number of ongoing partners different than predicted at baseline, was -0.28 overall, ranging from -1.91 to -0.41 for MSM with any ongoing partnerships at baseline. Comparing MSM of the same baseline degree, the level of bias was stronger for black compared with white MSM, and for younger compared with older MSM.
Conclusions. Research studies may overestimate degree when it is quantified cross-sectionally. Adjustment and structured sensitivity analyses may account for bias in studies of human immunodeficiency virus or sexually transmitted infection prevention interventions.
Network Drivers of Infectious Disease Dynamics
The configuration of sexual networks within a population plays a critical role in the spread of HIV and other sexually transmitted infections, yet characterizing the structure of dynamic networks in which epidemiologically relevant partnerships form and dissolve over time is challenging. Recent developments in statistics (temporal exponential random graph models), however, have yielded important new methods to allow for the recontruction and simulation of dynamic contact networks from easily collected data. These methods allow for testing hypotheses about the relationship between network configurations and transmission risk in innovative ways.
One of my focal research interests is to characterize how network structures are drivers of infectious disease transmission broadly. This research area began with my work on the impact of concurrency on HIV transmission in heterosexual partnership networks in sub-Saharan Africa. Subsequently, I collaborated on research using a network framework to understand the causes of racial disparities in HIV among MSM. Work in this domain also involved hospital-acquired and respiratory infectious diseases, using both mathematical and statistical modeling approaches.
Representative Publications
Jenness SM, Goodreau SM, Morris M, Cassels S. Effectiveness of Combination Packages for HIV-1 Prevention in Sub-Saharan Africa Depends on Partnership Network Structure Sexually Transmitted Infections. 2016; 92: 619–624.

Objectives. Combination packages for HIV prevention can leverage the effectiveness of biomedical and behavioural elements to lower disease incidence with realistic targets for individual and population risk reduction. We investigated how sexual network structures can maximise the effectiveness of a package targeting sexually active adults in sub-Saharan Africa (SSA) with intervention components for medical male circumcision (MMC) and sexual partnership concurrency (having >1 ongoing partner).
Methods. Network-based mathematical models of HIV type 1 (HIV-1) transmission dynamics among heterosexual couples were used to explore how changes to MMC alone and in combination with changes to concurrency impacted endemic HIV-1 prevalence and incidence. Starting from a base model parameterised from empirical data from West Africa, we simulated the prevalence of circumcision from 10% to 90% and concurrency was modelled at four discrete levels corresponding to values observed across SSA.
Results. MMC and concurrency could contribute to the empirical variation in HIV-1 disease prevalence across SSA. Small reductions in concurrency resulted in large declines in HIV-1 prevalence. Scaling up circumcision in low-concurrency settings yields a greater relative benefit, but the absolute number of infections averted depends on both the circumcision coverage and baseline incidence. Epidemic extinction with this package will require substantial scale-up of MMC in low-concurrency settings.
Conclusions. Dynamic sexual network structure should be considered in the design and targeting of MMC within combination HIV-1 prevention packages. Realistic levels of coverage for these packages within southern Africa could lead to a reduction of incidence to the low levels observed in western Africa, and possibly, epidemic extinction.
Goodreau SM, Rosenberg ES, Jenness SM, Luisi N, Stansfield SE, Millett G, Sullivan P. Sources of Racial Disparities in HIV Prevalence among Men Who Have Sex with Men in Atlanta, GA: A Modeling Study. Lancet HIV. 2017; 4(7): e311-e3320.
 Background. In the USA, men who have sex men (MSM)
are at high risk for HIV, and black MSM have a substantially higher
prevalence of infection than white MSM. We created a simulation model
to assess the strength of existing hypotheses and data that account
for these disparities.
Background. In the USA, men who have sex men (MSM)
are at high risk for HIV, and black MSM have a substantially higher
prevalence of infection than white MSM. We created a simulation model
to assess the strength of existing hypotheses and data that account
for these disparities.
Methods. We built a dynamic, stochastic, agent-based network model of black and white MSM aged 18-39 years in Atlanta, GA, USA, that incorporated race-specific individual and dyadic-level prevention and risk behaviours, network attributes, and care patterns. We estimated parameters from two Atlanta-based studies in this population (n=1117), supplemented by other published work. We modelled the ability for racial assortativity to generate or sustain disparities in the prevalence of HIV infection, alone or in conjunction with scenarios of observed racial patterns in behavioural, care, and susceptibility parameters.
Findings. Race-assortative mixing alone could not sustain a pre-existing disparity in prevalence of HIV between black and white MSM. Differences in care cascade, stigma-related behaviours, and CCR5 genotype each contributed substantially to the disparity (explaining 10·0%, 12·7%, and 19·1% of the disparity, respectively), but nearly half (44·5%) could not be explained by the factors investigated. A scenario assessing race-specific reporting differences in risk behaviour was the only one to yield a prevalence in black MSM (44·1%) similar to that observed (43·4%).
Interpretation. Racial assortativity is an inadequate explanation for observed disparities. Work to close the gap in the care cascade by race is imperative, as are efforts to increase serodiscussion and strengthen relationships among black MSM particularly. Further work is urgently needed to identify other sources of, and pathways for, this disparity, to integrate concomitant epidemics into models, and to understand reasons for racial differences in behavioural reporting.
Goldstein ND, Jenness SM, Tuttle D, Power M, Paul DA, Eppes SC. Evaluating a neonatal intensive care unit HRSA surveillance programme using agent-based network modeling. Journal of Hospital Infection. 2018; 100(3): 337–343.
Background. Surveillance for meticillin-resistant Staphylococcus aureus (MRSA) in neonatal intensive care units (NICUs) is a commonplace infection prevention strategy, yet the optimal frequency with which to monitor the unit is unknown.
Aim. To compare various surveillance frequencies using simulation modelling.
Methods. One hundred NICU networks of 52 infants were simulated over a six-month period to assess MRSA transmission. Unit-wide surveillance occurred every N weeks where N={1,2,3,4}, and was compared with the current NICU policy of dynamic surveillance (i.e. weekly when at least one positive screen, otherwise every three weeks). For each surveillance period, colonized infants received a decolonization regimen (56% effective) and were moved to isolation rooms, if available.
Findings. As the surveillance frequency increased, the mean number of MRSA-colonized infants decreased, from a high of 2.9 (four-weekly monitoring) to a low of 0.6 (weekly monitoring) detected per episode. The mean duration of colonization decreased from 307 h (four-weekly monitoring) to 61 h (weekly monitoring). Meanwhile, the availability of isolation rooms followed an inverse relationship: as surveillance frequency increased, the availability of isolation rooms decreased (61% isolation success rate for four-weekly monitoring vs 49% success rate for weekly monitoring). The dynamic policy performed similar to a biweekly programme.
Conclusion. An effective MRSA surveillance programme needs to balance resource availability with potential for harm due to longer colonization periods and opportunity for development of invasive disease. While more frequent monitoring led to greater use of a decolonization regimen, it also reduced the likelihood of isolation rooms being available.
Nelson KN, Gandhi NR, Mathema B, Lopman BA, Brust JC, Auld SC, Ismail N, Omar SV, Brown RS, Allana S, Campbell A, Moodley P, Mlisana K, Shah NS, Jenness SM. Modeling Missing Cases and Transmission Links in Networks of Extensively Drug-Resistant Tuberculosis in KwaZulu-Natal, South Africa. American Journal of Epidemiology. 2020; DOI: 10.1093/aje/kwaa028.

Abstract. Patterns of transmission of drug-resistant tuberculosis (TB) remain poorly understood, despite over half a million incident cases worldwide in 2017. Modeling TB transmission networks can provide insight into drivers of transmission, but incomplete sampling of TB cases can pose challenges for inference from individual epidemiologic and molecular data. We assessed the effect of missing cases on a transmission network inferred from Mycobacterium tuberculosis sequencing data on extensively drug-resistant TB cases in KwaZulu-Natal, South Africa, diagnosed in 2011-2014. We tested scenarios in which cases were missing at random, missing differentially by clinical characteristics, or missing differentially by transmission (i.e., cases with many links were under- or oversampled). Under the assumption that cases were missing randomly, the mean number of transmissions per case in the complete network needed to be larger than 20, far higher than expected, to reproduce the observed network. Instead, the most likely scenario involved undersampling of high-transmitting cases, and models provided evidence for super-spreading. To our knowledge, this is the first analysis to have assessed support for different mechanisms of missingness in a TB transmission study, but our results are subject to the distributional assumptions of the network models we used. Transmission studies should consider the potential biases introduced by incomplete sampling and identify host, pathogen, or environmental factors driving super-spreading.
Models to Support HIV/STI Prevention Guidelines
Using my EpiModel software and novel network data streams, a primary focus of my applied modeling is to evaluate the optimal design of guidelines for the prevention and control of HIV and other sexually transmitted infections. For HIV PrEP, this work includes a model of the CDC guidelines given uncertainty of coverage and adherence, a race-stratified continuum model that addresses national HIV disparities reduction indicators, and potential integration of long-acting formulations into clinical practice. I have also evaluated the impact of making CDC STI screening guidelines more specific with regards to screening coverage and frequency.
Recently completed work has responded to new national policies and initiatives, using methodologically integrative approaches that more directly support public health decision making. This includes my 2020 study that evaluated the “Ending the HIV Epidemic” initiative, where we identified the need to address the mechanistic overlap between HIV prevention and treatment services. We have also completed a combined epidemic and economic budget optimization model that estimates the optimal spending strategies on clinical interventions to improve PrEP initiation and adherence.
Representative Publications
Jenness SM, Goodreau SM, Rosenberg E, Beylerian EN, Hoover KW, Smith DK, Sullivan PS. Impact of CDC’s HIV Pre-Exposure Prophylaxis Guidelines among MSM in the United States. Journal of Infectious Diseases. 2016; 214(12): 1800–1807.
Background. Preexposure prophylaxis (PrEP) is effective for preventing human immunodeficiency virus (HIV) infection among men who have sex with men (MSM) within trial settings. Population impact will depend on clinical indications for PrEP initiation, coverage levels, and drug adherence. No modeling studies have estimated the impact of clinical practice guidelines for PrEP issued by the Centers for Disease Control and Prevention (CDC).
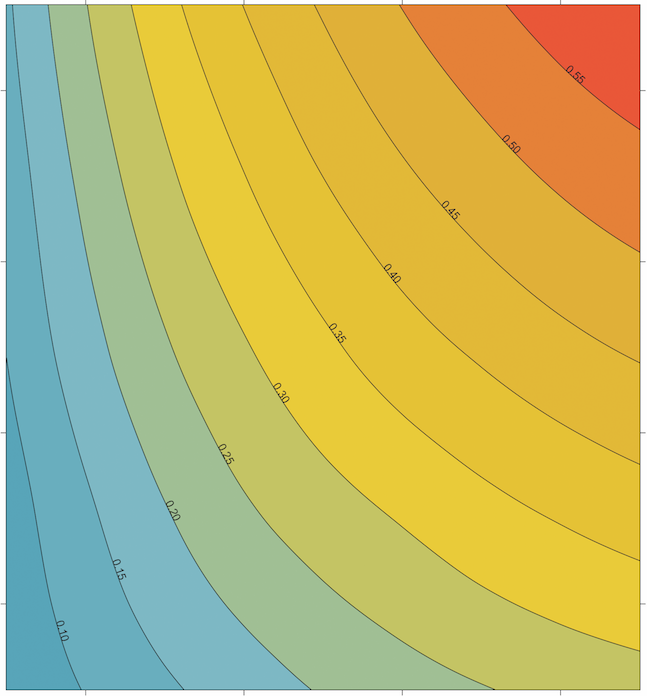
Methods. Mathematical models of HIV transmission among MSM were used to estimate the percentage of infections averted (PIA) and the number needed to treat (NNT) under behavioral indications of the CDC's PrEP guidelines. We modeled the contribution of these indications while varying treatment coverage and adherence.
Results. At 40% coverage of indicated MSM over the next decade, application of CDC guidelines would avert 1162 infections per 100 000 person-years, 33.0% of expected infections. The predicted NNT for the guidelines would be 25. Increasing coverage and adherence jointly raise the PIA, but reductions to the NNT were associated with better adherence only.
Conclusions. Implementation of CDC PrEP guidelines would result in strong and sustained reductions in HIV incidence among MSM in the United States. The guidelines strike a good balance between epidemiological impact (PIA) and efficiency (NNT) at plausible scale-up levels. Adherence counseling could maximize public health investment in PrEP by decreasing the NNT.
Shiny Web AppJenness SM, Maloney K, Smith SK, Hoover KW, Rosenberg ES, Goodreau SM, Weiss KM, Liu AY, Rao D, Sullivan PS. Addressing Gaps in HIV Preexposure Prophylaxis Care to Reduce Racial Disparities in HIV Incidence in the United States. American Journal of Epidemiology. 2019; Published online ahead of print.

Abstract. The potential for human immunodeficiency virus (HIV) preexposure prophylaxis (PrEP) to reduce the racial disparities in HIV incidence in the United States might be limited by racial gaps in PrEP care. We used a network-based mathematical model of HIV transmission for younger black and white men who have sex with men (BMSM and WMSM) in the Atlanta, Georgia, area to evaluate how race-stratified transitions through the PrEP care continuum from initiation to adherence and retention could affect HIV incidence overall and disparities in incidence between races, using current empirical estimates of BMSM continuum parameters. Relative to a no-PrEP scenario, implementing PrEP according to observed BMSM parameters was projected to yield a 23% decline in HIV incidence (hazard ratio = 0.77) among BMSM at year 10. The racial disparity in incidence in this observed scenario was 4.95 per 100 person-years at risk (PYAR), a 19% decline from the 6.08 per 100 PYAR disparity in the no-PrEP scenario. If BMSM parameters were increased to WMSM values, incidence would decline by 47% (hazard ratio = 0.53), with an associated disparity of 3.30 per 100 PYAR (a 46% decline in the disparity). PrEP could simultaneously lower HIV incidence overall and reduce racial disparities despite current gaps in PrEP care. Interventions addressing these gaps will be needed to substantially decrease disparities.
Maloney KM, Driggers R, Sarkar S, Anderson EA, Malik AA, Jenness SM. Projected Impact of Concurrently Available Long-Acting Injectable and Daily-Oral HIV Pre-Exposure Prophylaxis: A Mathematical Model. Journal of Infectious Diseases. 2020; 188(4): 743–752.
Background. Long-acting injectable HIV pre-exposure prophylaxis (LAI-PrEP) is reportedly efficacious, although full trial results have not been published. We used a dynamic network model of HIV transmission among men who have sex with men (MSM) to assess the population impact of LAI-PrEP when available concurrently with daily-oral (DO) PrEP.
Methods. The reference model represents the current HIV epidemiology and DO-PrEP coverage (15% among indicated) among MSM in the southeastern US. Primary analyses investigated varied PrEP uptake and proportion selecting LAI-PrEP. Secondary analyses evaluated uncertainty in pharmacokinetic efficacy and LAI-PrEP persistence relative to DO-PrEP
Results. Compared to the reference scenario, if 50% chose LAI-PrEP, 4.3% (95% SI: -7.3%, 14.5%) of infections would be averted over 10 years. LAI-PrEP impact is slightly greater than the DO-PrEP only regimen based on assumptions of higher adherence and partial protection after discontinuation. If the total PrEP initiation rate doubled, 17.1% (95% SI: 6.7%,26.4%) of infections would be averted. The highest population-level impact occurred when LAI-PrEP uptake and persistence improved
Conclusions. If LAI-PrEP replaces DO-PrEP, its availability will modestly improve the population impact. LAI-PrEP will make a more substantial impact if its availability drives higher total PrEP coverage, or if persistence is greater for LAI-PrEP.
Weiss KM, Jones JS, Anderson EJ, Gift T, Chesson H, Bernstein K, Workowski K, Tuite A, Rosenberg ES, Sullivan PS, Jenness SM. Optimizing Coverage versus Frequency for Sexually Transmitted Infection Screening of Men Who Have Sex with Men. Open Forum Infectious Diseases. 2019; 6(10): ofz405.
Background. The incidence of bacterial sexually transmitted infections (STIs) in men who have sex with men (MSM) has increased substantially despite availability of effective antibiotics. The US Centers for Disease Control and Prevention (CDC) recommends annual screening for all sexually active (SA) MSM and more frequent screening for high-risk (HR) MSM. The population-level benefits of improved coverage vs increased frequency of STI screening among SA vs HR MSM are unknown.
Methods. We used a network transmission model of gonorrhea (NG) and chlamydia (CT) among MSM to simulate the implementation of STI screening across different scenarios, starting with the CDC guidelines at current coverage levels. Counterfactual model scenarios varied screening coverage and frequency for SA MSM and HR MSM (MSM with multiple recent partners). We estimated infections averted and the number needed to screen to prevent 1 new infection.
Results. Compared with current recommendations, increasing the frequency of screening to biannually for all SA MSM and adding some HR screening could avert 72% of NG and 78% of CT infections over 10 years. Biannual screening of 30% of HR MSM at empirical coverage levels for annual SA screening could avert 76% of NG and 84% of CT infections. Other scenarios, including higher coverage among SA MSM and increasing frequency for HR MSM, averted fewer infections but did so at a lower number needed to screen.
Conclusions. The optimal screening scenarios in this model to reduce STI incidence among MSM included more frequent screening for all sexually active MSM and higher coverage of screening for HR men with multiple partners.
Prevention Response to the HIV and Bacterial STI Interaction
Although the interaction between STIs and HIV has been well-characterized, I have brought a network science and mathematical modeling framework to understanding the pressing issues in this domain. This is best represented by my model of the impact of HIV PrEP on STI incidence among MSM, which has recently led to empirical work characterizing the variability in the comprehensiveness of PrEP-based STI screening in this population. I have also led network-based modeling research that evaluates, in the opposite direction, the causal pathway from prevalent STIs to HIV acquisition and the potential caveats of partner-driven STI prevention strategies on missed opportunities for HIV prevention.
Representative Publications
Jenness SM, Weiss KM, Goodreau SM, Rosenberg E, Gift T, Chesson H, Hoover KW, Smith DK, Liu AY, Sullivan P. Incidence of Gonorrhea and Chlamydia Following HIV Preexposure Prophylaxis among Men Who Have Sex with Men. Clinical Infectious Diseases. 2017; 65(5): 712-18.
Background. Preexposure prophylaxis (PrEP) is highly effective for preventing human immunodeficiency virus (HIV) infection, but risk compensation (RC) in men who have sex with men (MSM) raises concerns about increased sexually transmitted infections (STIs). The Center for Disease Control and Prevention's (CDC's) PrEP guidelines recommend biannual STI screening, which may reduce incidence by treating STIs that would otherwise remain undiagnosed. We investigated these two counteracting phenomena.
Methods. With a network-based mathematical model of HIV, Neisseria gonorrhoeae (NG), and Chlamydia trachomatis (CT) transmission dynamics among MSM in the United States, we simulated PrEP uptake following the prescription indications and HIV/STI screening recommendations in the CDC guidelines. Scenarios varied PrEP coverage (the proportion of MSM indicated for PrEP who received it), RC (a reduction in the per-act probability of condom use), and the STI screening interval.
Results. In our reference scenario (40% coverage, 40% RC), 42% of NG and 40% of CT infections would be averted over the next decade. A doubling of RC would still result in net STI prevention relative to no PrEP. STIs declined because PrEP-related STI screening resulted in a 17% and 16% absolute increase in the treatment of asymptomatic and rectal STIs, respectively. Screening and timely treatment at quarterly vs biannual intervals would reduce STI incidence an additional 50%.
Conclusions. Implementation of the CDC PrEP guidelines while scaling up PrEP coverage could result in a significant decline in STI incidence among MSM. Our study highlights the design of PrEP not only as antiretroviral medication but as combination HIV/STI prevention incorporating STI screening.
Chandra C, Weiss KM, Kelley CF, Marcus JL, Jenness SM. Gaps in Screening of Sexually Transmitted Infections among Men Who Have Sex with Men during PrEP Care in the United States. Clinical Infectious Diseases. 2020; Published online ahead of print.
Background. The U.S. Centers for Disease Control and Prevention (CDC) recommends comprehensive sexually transmitted infection (STI) screening every 3-6 months for men who have sex with men (MSM) using HIV preexposure prophylaxis (PrEP). The gaps between these recommendations and clinical practice by region have not been quantified.
Methods. We used survey data collected from the internet-based ARTnet study between 2017 and 2019 on STI screening among MSM across the U.S., stratified by current, prior, and never PrEP use. Poisson regression models with robust error variance were used to model factors, including residence in the Southeast, associated with consistent ("always" or "sometimes") exposure site-specific STI screening during PrEP care.
Results. Of 3259 HIV-negative MSM, 19% were currently using PrEP, 6% had used PrEP in the past, and 75% had never used PrEP. Among ever PrEP users, 87%, 78%, 57%, and 64% reported consistent screening for STIs by blood sample, urine sample or urethral swab, rectal swab, or pharyngeal swab, respectively, during PrEP care. Compared to PrEP users in all other regions, PrEP users in the Southeast were significantly less likely to be consistently screened for urogenital (adjusted prevalence ratio [aPR], 0.86; 95% confidence interval [CI], 0.76-0.98) and rectal STIs (aPR, 0.76; 95% CI, 0.62-0.93) during PrEP care.
Conclusions. Substantial gaps exist between CDC recommendations for STI screening during PrEP care and current clinical practice, particularly for rectal and pharyngeal exposure sites that can harbor asymptomatic infections and for MSM in Southeast states where the STI burden is substantial.
Jones J, Weiss K, Mermin J, Dietz P, Rosenberg ES, Gift T, Chesson H, Sullivan PS, Lyles C, Bernstein K, Jenness SM. Proportion of Incident HIV Cases among Men Who Have Sex with Men Attributable to Gonorrhea and Chlamydia: A Modeling Analysis. Sexually Transmitted Diseases. 2019; 46(6): 357–363.

Background. Sexually transmitted infections (STIs) are associated with an increased risk of human immunodeficiency virus (HIV) acquisition and transmission. We estimated the proportion of HIV incidence among men who have sex with men attributable to infection with the 2 most common bacterial STIs, Neisseria gonorrhoeae (NG) and Chlamydia trachomatis (CT).
Methods. We used a stochastic, agent-based model of a sexual network of MSM with cocirculating HIV, NG, and CT infections. Relative risk (RR) multipliers, specific to anatomic site of infection, modified the risk of HIV transmission and acquisition based on STI status. We estimated the effect of NG and CT on HIV incidence overall and on HIV acquisition and HIV transmission separately. Each scenario was simulated for 10 years. The population attributable fraction (PAF) was determined for each combination of RRs by comparing the incidence in the final year of a scenario to a scenario in which the RRs associated with NG and CT were set to 1.0.
Results. Overall, 10.2% (interquartile range [IQR], 7.9-12.4) of HIV infections were attributable to NG/CT infection. Then in sensitivity analyses, the PAF for HIV transmission ranged from 3.1% (IQR, 0.5-5.2) to 20.4% (IQR, 17.8-22.5) and the PAF for HIV acquisition ranged from 2.0% (IQR, -0.7 to 4.3) to 13.8% (IQR, 11.7-16.0).
Conclusions. Despite challenges in estimating the causal impact of NG/CT on HIV risk, modeling is an alternative approach to quantifying plausible ranges of effects given uncertainty in the biological cofactors. Our estimates represent idealized public health interventions in which STI could be maximally prevented, setting targets for real-world STI interventions that seek to reduce HIV incidence.
Weiss KM, Jones J, Katz DA, Gift TL, Bernstein K, Workowski K, Rosenberg E, Jenness SM. Epidemiological Impact of Expedited Partner Therapy for Men Who Have Sex with Men: A Modeling Study. Sexually Transmitted Diseases. 2019; 46(11): 697–705.

Background. Expedited partner therapy (EPT) is an intervention for patients with gonorrhea or chlamydia, providing index patients with prescriptions or medication to give to their partners. Expedited partner therapy is recommended for heterosexuals but not for men who have sex with men (MSM), partially due to concerns about overtreatment of uninfected partners and missed opportunities for human immunodeficiency virus (HIV) diagnosis.
Methods. We extended our stochastic network-based mathematical model of HIV, gonorrhea, and chlamydia among MSM to include EPT. The EPT implementation was simulated for 10 years. Counterfactual scenarios varied EPT coverage, provision, uptake, and partnership window duration. We estimated sexually transmitted infection (STI) incidence, proportion of infections averted, and process outcomes under each scenario.
Results. Delivery of EPT to 20% of eligible MSM index patients (coverage) reduced cumulative STI incidence by 27% (interquartile range, 13%-39%) over 10 years compared with current estimated STI screening levels. A 20% increase in providing medication to non-index partners (provision) averted 32% (interquartile range, 20%-41%) of STI infections compared with estimated STI screening levels. When targeted by partnership type, EPT solely to casual partners maximized the population-level infections averted. The proportion of partners given medication who had no current STI varied from 52% to 63%, depending on coverage level. The proportion of partners given medication with undiagnosed HIV infection was 4% across scenarios.
Conclusions. Expedited partner therapy could reduce bacterial STI incidence for MSM. However, this intervention could result in missed opportunities for HIV/STI prevention and a substantial increase in use of antimicrobials by STI-uninfected MSM, raising concerns about cost and antimicrobial resistance.
Multi-Level Risk Factors for HIV and STI Acquisition
Understanding the etiology of infection for sexual transmitted infections is necessary to target disease prevention interventions towards at-risk persons. Transmission and acquisition risk have been particularly challenging to define within concentrated HIV epidemics where individual risk factors like recent multiple partnerships may be insufficient to fully characterize excesses in infection probability. My research in this domain has investigated the social, structural, and network-level factors for HIV/STI infection among key high-risk groups, including MSM in the United States and heterosexuals in both the US and Sub-Saharan Africa.
Representative Publications
Jenness SM, Begier E, Neaigus A, Murrill CS, Wendel T, Hagan H. Unprotected Anal Intercourse and Sexually Transmitted Diseases in High-Risk Heterosexual Women. American Journal of Public Health. 2011; 101(4): 745-750.

Objectives. We examined the association between unprotected anal intercourse and sexually transmitted diseases (STDs) among heterosexual women.
Methods. In 2006 through 2007, women were recruited from high-risk areas in New York City through respondent-driven sampling as part of the National HIV Behavioral Surveillance study. We used multiple logistic regression to determine the relationship between unprotected anal intercourse and HIV infection and past-year STD diagnosis.
Results. Of the 436 women studied, 38% had unprotected anal intercourse in the past year. Unprotected anal intercourse was more likely among those who were aged 30 to 39 years, were homeless, were frequent drug or binge alcohol users, had an incarcerated sexual partner, had sexual partners with whom they exchanged sex for money or drugs, or had more than 5 sexual partners in the past year. In the logistic regression, women who had unprotected anal intercourse were 2.6 times as likely as women who had only unprotected vaginal intercourse and 4.2 times as likely as women who had neither unprotected anal nor unprotected vaginal intercourse to report an STD diagnosis. We found no significant association between unprotected anal intercourse and HIV infection.
Conclusions. Increased screening for history of unprotected anal intercourse and, for those who report recent unprotected anal intercourse, counseling and testing for HIV and STDs would likely reduce STD infections.
Jenness SM, Hagan H, Wendel T, Murrill CS, Neaigus A, Gelpi-Acosta C. Reconsidering the Internet as an HIV/STD Risk for Men Who Have Sex with Men. AIDS & Behavior. 2010; 14(6): 1353-1361.

Previous studies linking online sexual partnerships to behavioral risks among men who have sex with men (MSM) may be subject to confounding and imprecise measurement of partnership-specific risks. We examined behavioral risks associated with having only online, only offline, or both online and offline partners in the past year, the confounding effects of multiple partnerships, and partnership-specific risks among a sample of MSM from New York City recruited offline in 2008. Overall, 28% of 479 participants had an online partner in the past year, but most of those (82%) also had an offline partner. Having an online partner was associated with past-year unprotected anal intercourse (UAI) and other risks, but not after controlling for multiple partnerships. There were slightly higher levels of risk within offline partnerships, but differences were largely attributable to MSM who had both offline and online partners. Last sex partners met offline were more likely to be HIV-serodiscordant and engage in concurrent substance use with the participant. This suggests that online partnerships may not be an independent cause of behavioral risks, but a marker for risks occurring independent of Internet use.
Jenness SM, Neaigus A, Hagan H, Murrill CS, Wendel T. HIV Infection and Sexual Partnerships between Injection Drug Users and Non-Injectors. AIDS Patient Care & STDS. 2010; 24(3): 175-181.

Sex partnerships with injection drug users (IDU) are an understudied network-level risk factor for heterosexual HIV infection. Heterosexuals with no history of injection were recruited from high-risk areas in New York City through respondent-driven sampling. We examined the prevalence of IDU sex partnerships among these non-IDU, the factors associated with having a past year IDU partner, and the independent association of HIV infection and IDU sex partnerships in multiple logistic regression. Of the 601 non-IDU in this analysis, 13.8% had a sex partner in the past year with a history of injection. IDU partnerships were significantly more common among women and those with higher levels of unprotected sex and drug and alcohol use. Overall, 7.0% tested positive for HIV. HIV prevalence was higher (p = 0.07) for participants with IDU partners (9.6%) compared to those with no IDU partners (4.6%). In multiple logistic regression, participants with IDU partners were over twice as likely to be HIV-infected (p = 0.08). Sex partnerships with IDU were common and may play an important role in heterosexual HIV transmission in areas with large IDU populations. Prevention interventions to encourage the disclosure of injection history and risk reduction specifically for those with IDU partners are indicated.
Methods for Unbiased Estimation in Survey Research
I have also been interested in the statistical and epidemiological methods for the estimation of characteristics of “hidden” populations, those who are difficult or impossible to sample with traditional probabilistic survey methods (e.g., random digit dialing and household-based recruitment). Two methods, respondent-driven sampling and venue-based sampling, have become increasingly popular both in the U.S. and internationally, but recent research suggests some systematic biases that impact statistical inference.
My research has investigated these biases among a large-scale venue-based study of men who have sex with men, and also the potential spatial bias within a respondent-driven sampling study of high-risk heterosexual adults in New York City. This work also involves using cross-sectional techniques to estimate HIV incidence, which may be only typically measured in expensive longitudinal cohorts.
Representative Publications
Jenness SM, Neaigus A, Murrill CS, Gelpi-Acosta C, Wendel T, Hagan H. Recruitment-Adjusted Estimates of HIV Prevalence and Risk Among Men Who Have Sex with Men: Effects of Weighting Venue-Based Sampling Data. Public Health Reports. 2011; 126(5): 635-642.

Objectives. We investigated the impact of recruitment bias within the venue-based sampling (VBS) method, which is widely used to estimate disease prevalence and risk factors among groups, such as men who have sex with men (MSM), that congregate at social venues.
Methods. In a 2008 VBS study of 479 MSM in New York City, we calculated venue-specific approach rates (MSM approached/MSM counted) and response rates (MSM interviewed/MSM approached), and then compared crude estimates of HIV risk factors and seroprevalence with estimates weighted to address the lower selection probabilities of MSM who attend social venues infrequently or were recruited at high-volume venues.
Results. Our approach rates were lowest at dance clubs, gay pride events, and public sex strolls, where venue volumes were highest; response rates ranged from 39% at gay pride events to 95% at community-based organizations. Sixty-seven percent of respondents attended MSM-oriented social venues at least weekly, and 21% attended such events once a month or less often in the past year. In estimates adjusted for these variations, the prevalence of several past-year risk factors (e.g., unprotected anal intercourse with casual/exchange partners, ≥5 total partners, group sex encounters, at least weekly binge drinking, and hard-drug use) was significantly lower compared with crude estimates. Adjusted HIV prevalence was lower than unadjusted prevalence (15% vs. 18%), but not significantly.
Conclusions. Not adjusting VBS data for recruitment biases could overestimate HIV risk and prevalence when the selection probability is greater for higher-risk MSM. While further examination of recruitment-adjustment methods for VBS data is needed, presentation of both unadjusted and adjusted estimates is currently indicated.
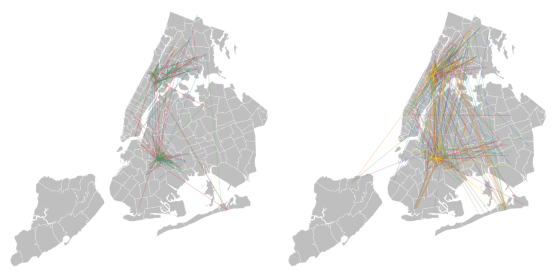
Jenness SM, Neaigus A, Wendel T, Gelpi-Acosta C, Hagan H. Spatial recruitment bias in respondent-driven sampling: Implications for HIV prevalence estimation in urban heterosexuals. AIDS & Behavior. 2014; 18(12): 2366-73.

Respondent-driven sampling (RDS) is a study design used to investigate populations for which a probabilistic sampling frame cannot be efficiently generated. Biases in parameter estimates may result from systematic non-random recruitment within social networks by geography. We investigate the spatial distribution of RDS recruits relative to an inferred social network among heterosexual adults in New York City in 2010. Mean distances between recruitment dyads are compared to those of network dyads to quantify bias. Spatial regression models are then used to assess the impact of spatial structure on risk and prevalence outcomes. In our primary distance metric, network dyads were an average of 1.34 (95 % CI 0.82–1.86) miles farther dispersed than recruitment dyads, suggesting spatial bias. However, there was no evidence that demographic associations with HIV risk or prevalence were spatially confounded. Therefore, while the spatial structure of recruitment may be biased in heterogeneous urban settings, the impact of this bias on estimates of outcome measures appears minimal.
Jenness SM, Neaigus A, Murrill CS, Gelpi-Acosta C, Wendel T, Hagan H. Estimated HIV Incidence among High-Risk Heterosexuals in New York City, 2007. Journal of Acquired Immune Deficiency Syndrome. 2011; 56(2): 193-197.

Estimates of HIV incidence rates among high-risk heterosexuals (HRH) in the United States have been limited to heterosexual subgroups like prison inmates and commercial sex workers. In this analysis, we estimate incidence with detuned assay testing among a group of HRH defined through a multidimensional sampling strategy and recruited through respondent-driven sampling. Incidence was 3.31% per year (95% confidence interval = 1.43 to 6.47) overall and 2.59% per year (95% confidence interval = 0.84 to 6.06) among participants with no lifetime history of drug injection or male-to-male sex. This study design is suggested as an efficient method for recruiting HRH for cohort studies and behavioral interventions.
Demographic Dynamics & Infectious Disease
With Susan Cassels, we are currently investigating the implications of migration and mobility on HIV transmission dynamics within an urban slum neighborhood in Accra, Ghana. This research involved primary data collection during the summer of 2012, in which we conducted a household-based cross-sectional study of sexually active adults. Study procedures included a detailed structured survey and a diagnostic HIV-1/2 test. In addition to the main probability sample, a secondary sample of cohabiting sexual partners were recruited, with data linkages to the main survey.
Our goal is to use traditional statistical analysis and stochastic mathematical modeling to investigate the relationships between migration/mobility, sexual partner concurrency, and HIV transmission in Ghana and other West African countries. We are also interesting in discussing and developing the methods for epidemiological research in populations with high rates of demographic turnover, as measuring disease prevalence and risk factors becomes complicated in highly-mobile or high-mortality areas.
Representative Publications
Cassels S, Jenness SM, Biney AA, Ampofo WK, Dodoo RN. Migration, sexual networks, and HIV in Agbogbloshie, Ghana. Demographic Research. 2014; 31: 861-888.
Background. HIV is spread through structured sexual networks, which are influenced by migration patterns, but network-oriented studies of mobility and HIV risk behavior have been limited.
Objectives. We present a comprehensive description and initial results from our Migration & HIV in Ghana (MHG) study in Agbogbloshie, an urban slum area within Accra, Ghana.
Methods. The MHG study was a population-based cross-sectional study of adults aged 18-49 in Agbogbloshie in 2012. We used a one-year retrospective relationship history calendar to collect egocentric network data on sexual partners as well as migration and short-term mobility, and tested for prevalent HIV-1/2 infection.
Results. HIV prevalence was 5.5%, with prevalence among women (7.2%) over twice that of men (2.8%). Three-quarters of residents were born outside the Greater Accra region, but had lived in Agbogbloshie an average of 10.7 years. Only 7% had moved housing structures within the past year. However, short-term mobility was common. Residents had an average of 7.3 overnight trips in the last year, with women reporting more travel than men. Thirty-seven percent of men and 9% of women reported more than one sexual partner in the last year.
Conclusions. Population-based surveys of migration and sexual risk behavior using relationship history calendars in low-resource settings can produce high quality data. Residents in Agbogbloshie are disproportionately affected by HIV, and have high levels of short-term mobility. HIV prevention interventions targeted to highly mobile populations in high prevalence settings may have far-reaching and long-term implications.
Cassels S, Jenness SM, Khanna AS. Conceptual framework and research methods for migration and HIV transmission dynamics. AIDS & Behavior. 2014; 18(12): 2302-13.

Migration and mobility have had a profound influence on the global HIV epidemic. We propose a network-dyadic conceptual model to interpret previous literature and inform the development of future research with respect to study design, measurement methods, and analytic approach. In this model, HIV transmission is driven by risk behaviors of migrants that emerges and is enabled by mobility, the bridging of sub-epidemics across space and time, and the displacement effects on the primary residential sending community for migrants. To investigate these causal pathways, empirical study designs must measure the relative timing of migratory events, sexual risk behaviors, and incident HIV infections. Network-based mathematical models using empirical data on partnerships help gain insight into the dynamic disease transmission systems. Although the network-dyadic conceptual model and related network methods may not address all questions related to migration and HIV, they provide a unified approach for future research on this important topic.